Year Two of the pandemic and mask-wearing has been a feature of daily routine and not likely to go anywhere any time soon. If your skin is suffering, the data tells us you’re certainly not alone.
54.5% of mask-wearers experience some sort of skin reaction.
Of these, acne is the most frequent (39.9%), followed by rashes on the face (18.4%), and itching (15.6%).
The upshot of the last two-years is there is now more research available detailing why MaskFace happens and how to best manage it.
But first, skin-friendly tips for mask-wearing
- Do not wear make-up at all on the skin covered by the mask.
- Choose a moisturiser with a balance of humectants (eg hyaluronic acid) to hydrate and ceramides to strengthen the barrier function.
- Rebalance your skin microbiome with topical probiotics.
- Change and or wash your mask as regularly as possible!
Masks and MaskFace
When you wear a mask, a unique microclimate is created according to the level of fresh airflow available to your skin. So, it makes sense that the higher-protection mask types impact the skin differently to lower-protection varieties.
For example, we know that surgical masks provide superior protection compared to cloth, but they’re also more likely to cause skin reactions.
Studies are also showing that N95 respirators – even higher-grade protection – are associated with more adverse skin reactions compared to surgical masks. This makes sense because N95s create a microenvironment that inhibits fresh air to the skin to keep pathogens out.
How long do you wear it?
Duration of wear is also a contributing factor.
Studies tell us that wearing a mask for more than four hours per day increases stress on the skin. Re-using (dirty) masks also increases the likelihood of adverse skin reactions.
What is happening to your skin under the mask?
Short duration wear: Wearing a mask for short periods causes the skin to get hotter, redder and oilier while simultaneously losing hydration. According to a 2021 study from South Korea, in only one hour the skin around the mouth and nose is most adversely affected.
Long duration wear: This is the reality for essential workers: extended periods, often in high-protection face masks. Another study from South Korea analysed skin changes over 6‐months of daily, continuous mask wear. The study compared changes to the skin underneath the mask to “non-masked” skin on the forehead over the same period and found that long‐term mask wearing affected the skin barrier and dryness.
In the “mask‐skin zone”, trans-epidermal water loss (TEWL) increased but skin hydration decreased, indicating impairment in the skin barrier function.
These changes in TEWL and skin hydration were thought to be related to the increased amount of surface skin keratin and the increase in pores that were also found over this 6-month period in the mask-skin zone. Skin elasticity of the mask‐skin zone also reduced as the skin dried out.
The result is “Mask Face” where the skin under the mask gets:
Drier and more sensitive = Maskitis.
OR
Oily and irritated = Maskne.
Let’s talk about Maskne
“Maskne” was coined in 2020 during the early days of the COVID-19 pandemic.
Consistent mask wear creates an occlusive skin microenvironment that leads to increased oil production and changes in the skin’s natural microbiome. Added to this is friction from the mask against the skin, et voila: you have an acne flare up. For acne-prone populations (active, young adults; oily skin types; those with genetic predisposition) humidity, and outdoor mask wearing (increased sweating) are triggering factors for Maskne.
Clinical criteria proposed for the diagnosis of Maskne are:
- onset of acne within six (6) weeks of regular face mask wear. OR
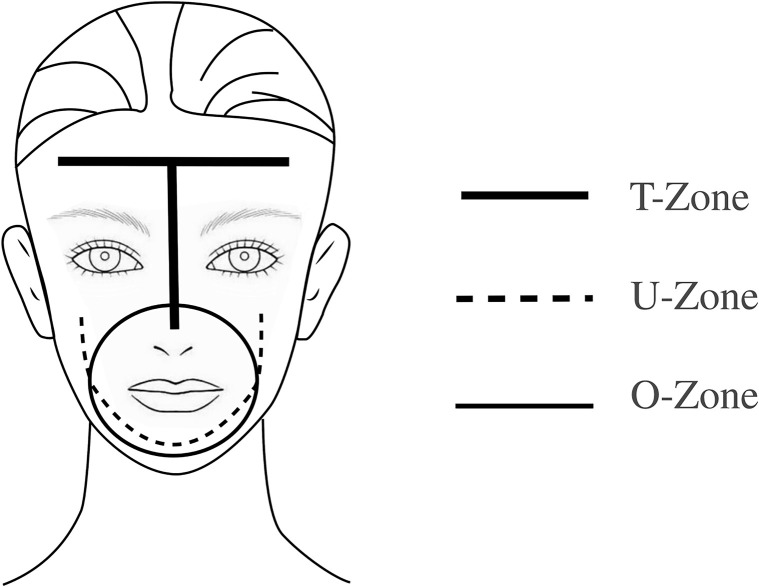
- exacerbation of acne in the masked area in a distinct pattern, referred to as the O-zone (see fig1)
How to manage Maskne
Managing this type of acne flare-up requires special consideration because even though your skin is oilier, the skin’s barrier function is impaired by the increased TEWL and reduced hydration, so it is more sensitive than normal.
Your usual skin care routine may be too harsh and cause more problems.
Switching to an oil-based cleanser is likely to be helpful. Oil cleansers regulate oil production while simultaneously increasing hydration of the skin. It’s a win-win! Our personal faves at SkinBox are Universkin’s O Cleanser or the Perfect Cleaning Oil by Paula’s Choice.
If an oil cleanser is not for you, try a gentle, foaming cleanser with antibacterial properties, such as this cleansing bar from Cetaphil ®
If you use a topical retinoid (Vitamin A), you may need to reduce the strength or frequency of use while your barrier function is impaired.
Think of your skin as a brick wall and the skin cells as the bricks. When barrier function is impaired, it is like cracks appearing in the cement holding the wall together so more “stuff” (good and bad!) can penetrate deeper into the wall.
dr sarah boxley
So, less active ingredient may actually be more helpful in this situation, as the amount that is getting in is proportionally more.
The plan of attack
Niacinamide: Amp up your niacinamide (Vitamin B3). Niacinamide has anti-inflammatory, antimicrobial, sebostatic and antipruritic effects so it will help soothe the skin, stop it itching, make it less oily and regulate the bacteria living there. Head-to-head studies of 4% niacinamide with 1% clindamycin gel (a prescription-only medication) have shown they are equally effective in mild-moderate acne at reducing pustules, comedones and papules.
Zinc Salts: Zinc salts (sulphate and gluconate), have been shown to have antibacterial and anti-inflammatory effects when applied to the skin and may also decrease oil production. (It is possible to add zinc sulphate to a customised serum when we make this in-clinic).
Topical Probiotics: When it comes to regulating the microbiome: the balance of bacteria that are naturally living on your skin, there are quite a few products on the market that can have a positive impact.
My personal fave is Dermiotic elixir from @synergieskin. “Adding a few drops to your daily routine is the skin equivalent of probiotics for your gut.”
dr Sarah Boxley
Learn more about how SkinBox custom creates skin formulas and routines for Maskne skin here:
Maskitis
Increased temperature under your mask can trigger sweat/heat-related dermatoses, and exacerbate chronic dermatoses such as perioral dermatitis, rosacea, and eczema. Your breath creates a little microclimate and further acts to dehydrate your own skin. As the skin dries out, the barrier function is impaired and the skin becomes increasingly irritated leading to redness, flaky and itchy skin with small red papules.
The plan of attack here is similar to maskne, but rather than reducing pimples, the focus is on reducing irritation and seriously ramping up your hydration.
The plan of attack
- Cleanse: Oil cleanser is an absolute godsend here. As well as using it to clean, you can also mix it in a 50:50 blend with hyaluronic acid serum to create an easy reparative face mask to leave on for 30 mins at the end of each day. Our particular favourites here at SkinBox are Universkin’s O Cleanser or the Perfect Cleaning Oil by Paula’s Choice.
If oil cleanser is just not your thing, try a gentle milky face wash instead, such as Synergie’s Biocleanse, Gel-to-Cream from Paula’s Choice, or Cerave Hydrating Cleanser
- Topical Probiotics: After cleansing, give your natural microbiome some love with a couple of drops of probiotic serum. A DIY alternative: make a puree of salted sauerkraut (not the sort in vinegar) and apply this as a mask for 30mins. It is not as convenient as drops from a bottle but good if you have lots of extra cabbages!
- Niacinamide: Then get our old friend niacinamide (vitamin B3)- the powerhouse of cosmeceutical skincare – in the mix. This is readily available in concentrations of up to 21% however, it is worth seeking professional advice rather than going in guns blazing because your skin may be better suited to a lower strength. In this situation, we are using vitamin B3 mainly to strengthen barrier function and boost water-holding skin lipids, as well as to calm & reduce inflammation. One of the lesser-known superpowers of niacinamide is its ability to increase skin ceramide levels, which are vital when it comes to preventing water loss.
- Exfoliate: The dry, dead top layer of skin needs to come off but most exfoliators are too harsh for skin that is this sensitive, and can irritate the skin even further.
Avoid physical scrubs, high concentrations of BHA or Vitamin A. Low concentration lactic acid is an option, but if this is still too much, a gentle acid-free exfoliating serum specifically designed for super-sensitive skin is probably your answer.
Our fave at SkinBox is Luciderm, which uses enzymes rather than acid to loosen and lift the dead skin cells.

- Hydrate: This is an absolute must. Now is not the time for fancy anti-aging moisturisers with heaps of chemical ingredients. Humectants (usually a bit pointless in Perth due to our weather & aircon) have a useful role here. These work by drawing moisture into themselves and holding it in the top layer of skin. Since the microenvironment under your mask is much more humid due to the moisture in your breath, you can use this to your advantage. Dr Sarah’s go-to moisturiser for super-dry, inflamed skin is this little beauty from Cerave – as well as hyaluronic acid, it has 3 different ceramides to strength and repair the barrier function and is incredibly cost-effective. Slather it on!
Learn more about how SkinBox custom creates skin formulas and routines for Maskitis skin here:
References:
Techasatian L, Lebsing S, Uppala R, Thaowandee W, Chaiyarit J, Supakunpinyo C, Panombualert S, Mairiang D, Saengnipanthkul S, Wichajarn K, Kiatchoosakun P, Kosalaraksa P. The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. J Prim Care Community Health. 2020 Jan-Dec;11:2150132720966167. doi: 10.1177/2150132720966167. PMID: 33084483; PMCID: PMC7786409.
Park SR, Han J, Yeon YM, Kang NY, Kim E, Suh BF. Long-term effects of face masks on skin characteristics during the COVID-19 pandemic. Skin Res Technol. 2021 Oct 19:10.1111/srt.13107. doi: 10.1111/srt.13107. Epub ahead of print. PMID: 34668244; PMCID: PMC8662003.
Park SR, Han J, Yeon YM, Kang NY, Kim E. Effect of face mask on skin characteristics changes during the COVID-19 pandemic. Skin Res Technol. 2021 Jul;27(4):554-559. doi: 10.1111/srt.12983. Epub 2020 Nov 20. PMID: 33217053; PMCID: PMC7753630.
Hua W, Zuo Y, Wan R, Xiong L, Tang J, Zou L, Shu X, Li L. Short-term skin reactions following use of N95 respirators and medical masks. Contact Dermatitis. 2020 Aug;83(2):115-121. doi: 10.1111/cod.13601. Epub 2020 Jun 8. PMID: 32406064; PMCID: PMC7272965.
Teo WL. The “Maskne” microbiome – pathophysiology and therapeutics. Int J Dermatol. 2021 Jul;60(7):799-809. doi: 10.1111/ijd.15425. Epub 2021 Feb 12. PMID: 33576511; PMCID: PMC8013758.
Teo WL. Diagnostic and management considerations for “maskne” in the era of COVID-19. J Am Acad Dermatol. 2021 Feb;84(2):520-521. doi: 10.1016/j.jaad.2020.09.063. Epub 2020 Oct 1. PMID: 33011321; PMCID: PMC7528820.
